What is a Letter of Medical Necessity and When do you Need one?
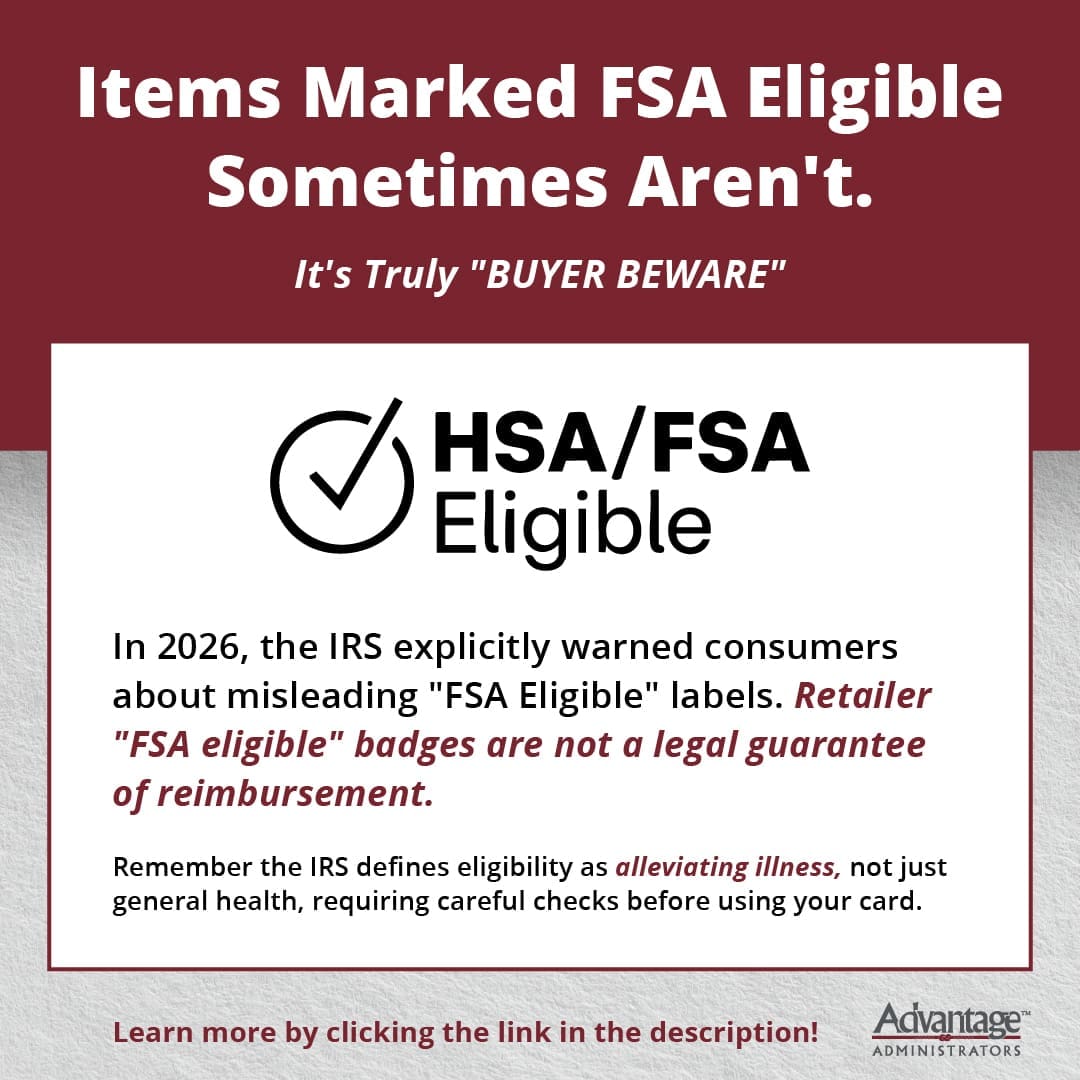
When it comes to using pre-tax health accounts like health savings accounts (HSAs), flexible spending accounts (FSAs) and health reimbursement arrangements (HRAs), you may assume that all medical expenses are automatically covered. However, certain expenses require additional documentation to be considered eligible. That’s where a letter of medical necessity (LMN) comes in.
If you’ve ever been told you need one or you’re wondering when it’s required, this guide will explain what an LMN is, why it’s important and how to obtain one.
What is a Letter of Medical Necessity?
A letter of medical necessity is a document written by a licensed healthcare provider that verifies a specific treatment, service or product that is medically necessary for a patient’s health. It’s typically required when an expense isn’t automatically deemed eligible under IRS guidelines but can be considered eligible with a doctor’s confirmation.
In simple terms, an LMN serves as proof that a treatment or item isn’t just for general wellness. It’s essential for managing a diagnosed medical condition.
When do you Need a Letter of Medical Necessity?
Not all healthcare expenses require an LMN but you’ll need one for certain treatments, services or items that are on the IRS’s “maybe” list—expenses that could be eligible if prescribed for a medical condition rather than for general health or personal preference.
Here are common examples of expenses that often require an LMN:
- Massage therapy – Covered if prescribed to treat a medical condition like chronic pain, not just for relaxation
- Nutritional counseling or special diets – Eligible if required for a medical condition like diabetes or celiac disease
- Gym memberships or exercise programs – Covered only if prescribed for a medical reason, such as cardiac rehabilitation or physical therapy
- Orthopedic shoes or inserts – May require an LMN to confirm they are needed for a foot or joint condition
- Weight loss programs – Eligible if prescribed by a doctor for a condition like obesity, hypertension or diabetes
- Alternative therapies (acupuncture, chiropractic care, etc.) – Often eligible but may require an LMN depending on the condition being treated
How to Obtain a Letter of Medical Necessity
If you need an LMN, follow these steps:
- Consult your healthcare provider – Ask your doctor, specialist or other licensed medical professional to write the letter. They must clearly state why the treatment, service or item is medically necessary for your condition.
- Ensure it includes key information – An LMN should include:
- Your name and diagnosis
- Recommended treatment, service or item
- A statement explaining why it’s medically necessary
- The provider’s name, credentials and signature
- Submit to your HSA, FSA or HRA administrator – Before making a purchase, check with your account provider to see if an LMN is required. If so, submit it as part of your reimbursement request or claims processes
How Long is an LMN Valid?
Most LMNs are valid for one year, though some plans may require renewal sooner. If you need ongoing treatment, check with your provider to ensure you have an up-to-date LMN each year.
The information in this blog post is for educational purposes only. It is not investment, legal or tax advice. For legal or tax advice, you should consult your own counsel. To stay up to date on benefits trends and insights, subscribe to our blog.





 Flex Plans
Flex Plans Forms
Forms HSA
HSA HRA
HRA Retirement
Retirement Health Shopper
Health Shopper FSA Store
FSA Store